My wish list
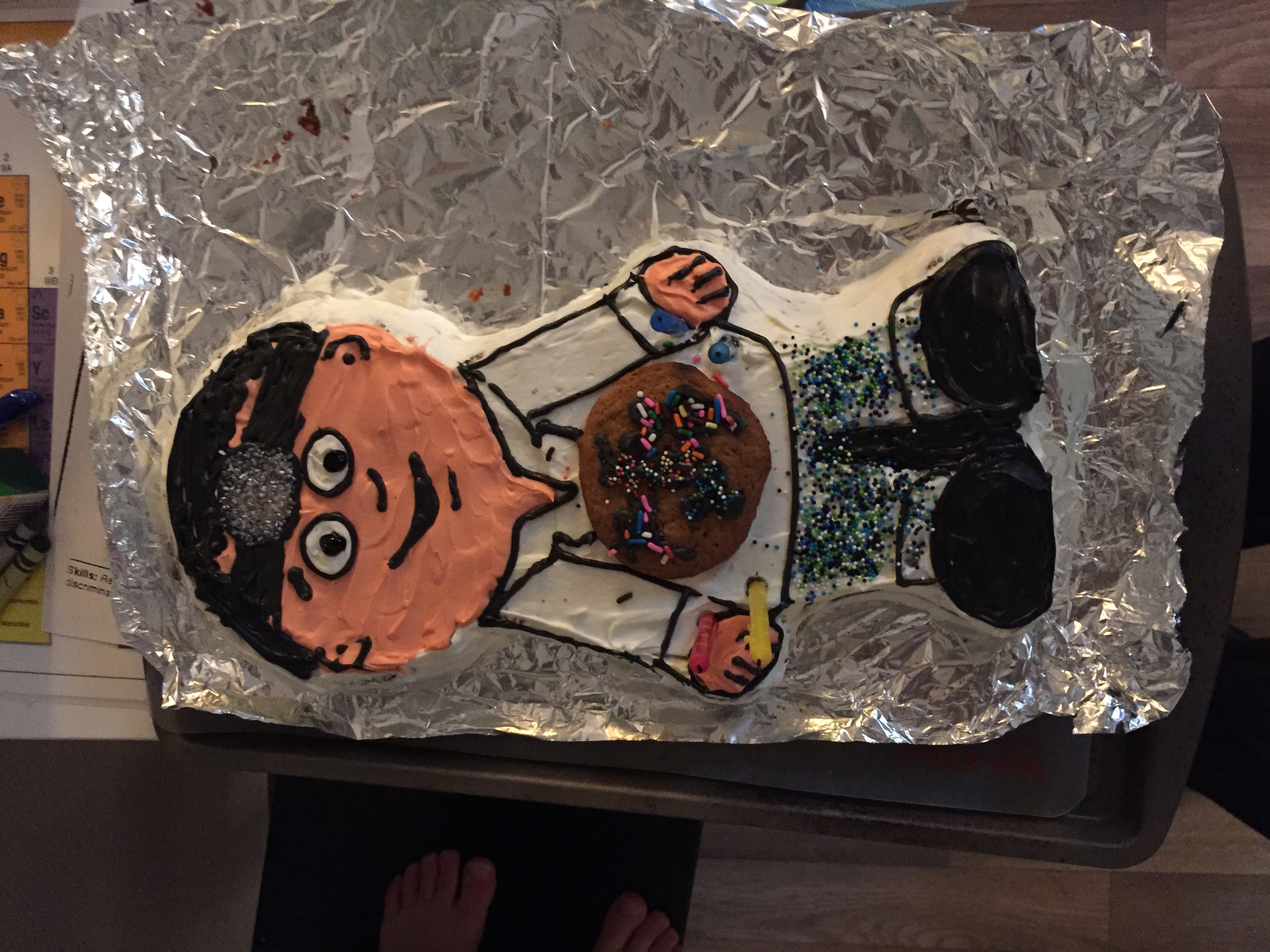
This week I celebrated my 39th birthday and though I got formal presents (none of which are pictured, but my cake and Petri dish cookie is), Ebola continued to "bless" us all with new gifts, including the 2nd Texas healthcare worker's infection and her unfortunate CDC-sanctioned travel.
As I argued in my recent Time op-ed, these healthcare worker infections in the US provide incontrovertible evidence that not every hospital is prepared to deal--as they should be--with all aspects of an Ebola patient's care. This evidence was not something I welcomed as I had been someone who was completely convinced Ebola would not have secondary spread within the US. This shattered belief of mine stemmed from the history of uneventful importations of Lassa Fever, Marburg, and MERS.
That healthcare workers who cared for the critically ill Thomas Eric Duncan are the ones who were infected, as opposed to his circle of direct contacts who are about to complete their quarantine periods, argues that the modern ICU environment, with its tubes, invasive procedures, and central venous lines, is a terrain that Ebola has found conducive to its spread. It may be the case that in ordinary (i.e. non-critical) cases of hospitalization, Ebola may be stymied.
This is a virus that remains less contagious than many others and has a restrained ability to spread between humans, save to caregivers (healthcare workers or others). However, the virus has evolved to exploit any lapse in the barrier precautions employed by those who are in its midst. These lapses can not occur for this is an unforgiving virus.
The first priority in ensuring that additional healthcare worker infections do not occur is to:
The cookie is a Petri dish of different bacteria
1. Stop this outbreak at its source--the head of the hydra is in West Africa and that is where the battle must be waged aggressively. The recently leaked WHO document illustrates how a gross initial underestimation of the outbreak's potential for spread in West Africa allowed this outbreak to fester longer and gain an incredible head start that transformed later interventions into mere squirt guns in the face of a raging forest fire.
2. Treat any additional imported or healthcare worker cases in the biocontainment facilities at the NIH, Emory, and Nebraska. Though scarce, these facilities have proved their adeptness at handling Ebola cases safely. This should be our 1st tier and hopefully will be able to absorb what will only be a trickle of imported cases.
3. Designate additional facilities in every region of the US that have some capacity to care for Ebola patients safely and can be used as 2nd tier facilities. These facilities must be thoroughly educated, drilled, and prepared to handle Ebola patients. Protocols and passive education will not be enough.
4. Dampen the panic that is now, understandably, widespread amongst the public through concise, clear communication based on scientific facts. Ruling out Ebola in every vomiting frat boy is unproductive and a poor use of resources.
5. Determine what the role of invasive interventions on Ebola patients should be going forward. It is likely that early recognition and treatment of Ebola patients with aggressive fluid resuscitation is essential and possibly able to forestall the dire complications that Mr. Duncan suffered. Is the benefit of such procedures as dialysis and mechanical ventilation outweighed by the risk to healthcare workers? Do such procedures actually improve outcomes?
All our actions to stop Ebola must be thoroughly informed by the facts and instantaneously integrated with any and all new discoveries that emerge. By facing this pathogen with active minds--mankind's ultimate resource and game-changer--it will be stopped.